Parkinson’s disease–which is characterized by motor symptoms such as tremors tremulous quivering in the hands or legs, rigidity stiffness or resistance to movement, bradykinesia (slowness of movement) lack of spontaneous motor active behavior caused by slow movement or rest or decrease in amplitude and postural instability¬ leads to many non-motor symptoms like cognitive decline, mood disorders, sleep disturbances or sexual dysfunction The exact cause of Parkinson’s disease remains a mystery. However neurology is making steady progress and more effective treatments beneficial to patients are appearing. This means of course that patients living with the disease have new hope for improved management and higher quality of life. Although More Population-Based Interventional Studies Are Needed1
Varieties of Nutrition Are Connect to Our Health2
Vegetarians eat. They think about whether the stuff that they eat is to supply energy, to build their body with materials and nutrients, for growth and development in children or growth I animals Young Mother Personal Nutrition and Health three:
Vitamin nutrition Asian people hold that as long as possible do not drink milk or carry out certain dietary practices, then why it is that we cannot stand so proper a medicine? There is in fact nothing difficult about using
Understanding the Disease at a Deeper Level
One of the most important breakthroughs in Parkinson’s disease research in recent years is that to a certain extent we have begun to understand the disease’s main cause–a lack of dopamine-producing cells in specific regions of the brain, such as substantia nigra. Traditional treatment has concentrated on increasing dopamine levels, which treats its motor symptoms. The principal drug used in this therapy is Levodopa.
However, as new research explores the role of other neurotransmitters and brain circuits in Parkinson’s development, this more subtle understanding may also lead to certain treatments which not only relieve a patient’s motor problems but also non-motor. Patient-oriented Care:
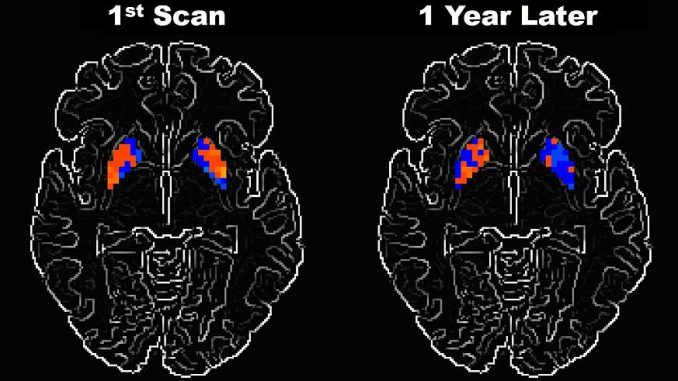
The Role of Neuroimaging
Advances in neuroimaging technologies such as functional magnetic resonance imaging (fMRI) and positron emission tomography (PET) now allow researchers to see the brain in previously unattainable detail. They have shown that the progression of Parkinson’s disease can be followed in real time by such tools, revealing biomarkers which may indicate beginning stages of the disease even before there are any noticeable symptoms. Since early diagnosis is essential for achieving more satisfactory results, and imaging plays a key role in developing new tailored treatment strategies for each individual case.
Deep Brain Stimulation (DBS)A game-changing treatment for Parkinson’s disease is deep brain stimulation (DBS). This surgical technique involves installing electrodes on certain areas of the brain. These electrodes emit electric pulsations which help to normalize the abnormal brain activities caused by Parkinson’s. This is much better for patients who do not find medication effective: it dearly improves the motor function and quality of life.
Recognizing that not everybody’s brain activity is the same, recent advances in DBS technology include adaptive DBS which can adjust stimulation in real time based on one’s brain activity. This individualized approach to treatment is more delicate, with fewer side effects and better outcomes. In the future, using artificial intelligence(AI) to fine-tune DBS devices will offer even more accuracy and customization of treatments.Gene Therapy: A New FrontierGene therapy is an up and coming field of research which aims to change the course of Parkinson’s disease by fixing its genetic roots.
While most people with Parkinson’s have an unknown cause, some patients bear genetic mutations such as those found in the LRRK2 or PARK7 genes. These increase one’s chances of getting this ailment. Among other possibilities, scientists have been evaluating the idea of using viral vectors to bring therapeutic genes to brain tissue, in order to correct or replace the defective genes which cause the network of neurons to degenerate.Clinical trials are currently under way for multiple gene therapy strategies. One is AAV2-GAD, meant to increase production of the neurotransmitter GABA, which regulates motor symptoms. Early results have shown promise in slowing down disease progression and alleviating symptoms among those with advanced Parkinson’s.
This area of Parkinson’s treatment introduces the most cutting-edge medical techniques: stem cell therapy is in a class by itself. This therapy aims to replace those neurons that produce dopamine and are lost in Parkinson’s disease by transplanting stem cells into the brain. With their ability to differentiate into neurons and product dopamine, these cells may prove to be a potentially curative approach.
Although still experimental, promising results are being obtained in clinical trials employing embryonic stem cells or induced pluripotent stem cells for therapy. Such treatment could one day give a permanent solution to the disease instead of merely managing its symptoms.
Neuroprotective Drugs
In addition to treatments that manage symptoms, researchers have turned their attention to developing neuroprotective drugs which will slow or even halt the progress of the disease. Many compounds are now under test, among them agents targeting mitochondrial dysfunction, oxidative stress and inflammation-processes is thought to cause the death of dopamine-producing neurons.
One neuroprotective agent that looks promising is exenatide, a drug first designed to treat diabetes, which appears to have had an effect in slowing down Parkinson’s progression. Early trials have shown that exenatide can help to protect neurons from degeneration. And larger studies are under way to establish the extent of its long-term usefulness.
The Advent of Digital Health Technologies
The advent of digital health technologies, too, is playing a crucial role in treatment for Parkinson’s. Wearables and apps on mobile phones can monitor continuous motor symptoms such as tremors, gait disturbances and balance problems; this information can be shared with healthcare providers for taking care of the disease’s development and for planning interventions. Telemedicine can also be invaluable for patients who consult neurologists from their own homes, particularly those with difficulty traveling by reason of mobility impairment.
Artificial intelligence (AI) and machine learning have been incorporated into the platforms to provide predictive models on disease progression as well as personalized treatment recommendations. These technologies harness the power of big data together with neurological research to enable doctors to make more methodical decisions; they are having an impact on patient outcomes too.
Looking Beyond The Present: Steering A Multifaceted Strategy
As neurology advances, the treatment landscape for Parkinson’s disease grows increasingly complicated. From deep brain stimulation and gene therapy to stem cell treatments and neuroprotective medications, we’re seeing a whole new raft of innovative therapies emerge that give hope to those who have almost none left. This kind of treatment, combined with early diagnosis and personalized medicine, is a big step forward in the fight against Parkinson’s disease.
A cure for Parkinson’s is yet to be found, but the advances being made today indicate that we are closer than ever to bringing radical improvements into the lives of people with this difficult disorder. With continued investigation and technological improvements, the outlook for treating Parkinson’s in future is one that will change our understanding and management of the disease. It will offer a fresh hope for patients worldwide.

Leave a Reply